Sweden: Pioneering Dignified Living for Seniors

Sweden stands out as a global leader in elder care, and it’s not just because of its beautiful landscapes or progressive culture. The Swedish government invests around 4.5% of its GDP in elder care, making sure older adults can access high-quality support. In 2024, new policies made it even easier for seniors to get help at home, allowing them to maintain independence while receiving assistance when needed. Technology has become a big part of Swedish elder care; things like remote health monitoring and digital communication tools help reduce isolation and keep people connected. According to the Swedish National Board of Health and Welfare, a remarkable 90% of seniors reported satisfaction with their care in 2024. Sweden’s local municipalities are also empowered to tailor services, so no two communities are exactly alike—making care more personal. With a growing population of people over 65, Sweden continues to adapt, focusing on prevention, healthy living, and dignity above all.
Norway: Community and Safety at the Heart

Norway’s elder care system is built on the idea that everyone deserves to feel safe and supported as they age. The country spends about 5% of its GDP on elder care, which covers everything from high-standard nursing homes to accessible home care. In 2023, Norway took concrete steps to reduce wait times for care, leading to a 15% drop in delays for nursing home placements. Community-based support is a hallmark here—neighbors and volunteers are often involved in helping older adults stay active and engaged. The Norwegian Institute of Public Health reported that 85% of seniors feel secure and well cared for, which is no small feat in a world where loneliness is a growing concern. Training for caregivers is taken seriously, and there’s ongoing investment in both people and infrastructure. Norway’s approach blends the warmth of community with the reliability of a strong welfare system.
Japan: Where Innovation Meets Tradition

Japan faces unique challenges, with nearly 30% of its population over 65—a higher proportion than anywhere else. To meet this challenge, Japan has rolled out a national long-term care insurance program that covers everything from home help to high-tech rehabilitation. By 2024, the number of certified care workers had increased by 20%, helping address shortages and improve care quality. The Ministry of Health, Labour and Welfare says that 80% of seniors wish to age in place, so there’s been a big expansion in community-based services. Japan is famous for using robots in caregiving—these machines help with lifting, companionship, and even exercise routines. Cultural respect for elders remains central, and the family’s role is supported, not replaced, by the system. The result is a blend of tradition and technology, with seniors’ comfort and autonomy at the forefront.
Denmark: Personalizing Care for Every Senior

Denmark’s elder care system is all about giving seniors the support that fits their individual needs. The country invests around 4.8% of its GDP into elder care, ensuring that services are both broad and deep. In 2025, Denmark introduced new quality guidelines for nursing homes, and the impact was immediate: resident satisfaction jumped by 10%. The Danish Health Authority found that 75% of seniors feel their needs are fully met, a testament to the system’s flexibility. Caregivers in Denmark are highly trained and receive ongoing education, which helps maintain high standards. There’s also strong coordination between health services and social supports, so seniors aren’t left to navigate complex systems alone. Denmark’s approach values independence, but there’s always a safety net for those who need extra help.
Finland: Focusing on Well-Being and Social Life

Finland’s elder care goes beyond just providing medical services—it focuses on the whole person. The country spends about 4.2% of its GDP on elder care, with a big emphasis on mental health and social connection. In 2024, Finland launched a national program to boost seniors’ participation in social activities, resulting in a 30% increase in engagement. The Finnish Institute for Health and Welfare found that seniors involved in these activities report much higher happiness and sense of purpose. Health services are well-integrated with social supports, so seniors don’t fall through the cracks. Community centers and clubs are everywhere, helping older adults build friendships and stay active. The result is a system that helps seniors thrive, not just survive.
Canada: Expanding Options and Support

Canada has been making major improvements in elder care, especially in the last few years. The government now spends about 3.9% of its GDP on elder care, with a growing focus on helping seniors stay at home as long as possible. In 2023, new funding made home care more accessible, boosting available resources by 25%. According to Statistics Canada, 70% of seniors say they’re satisfied with their care options—a number that’s been climbing steadily. There’s also a strong emphasis on culturally sensitive care, which is important in such a diverse country. Care providers receive regular training, and there are more checks to ensure quality. Canada’s elder care system is far from perfect, but it’s heading in the right direction, with more attention to both rural and urban needs.
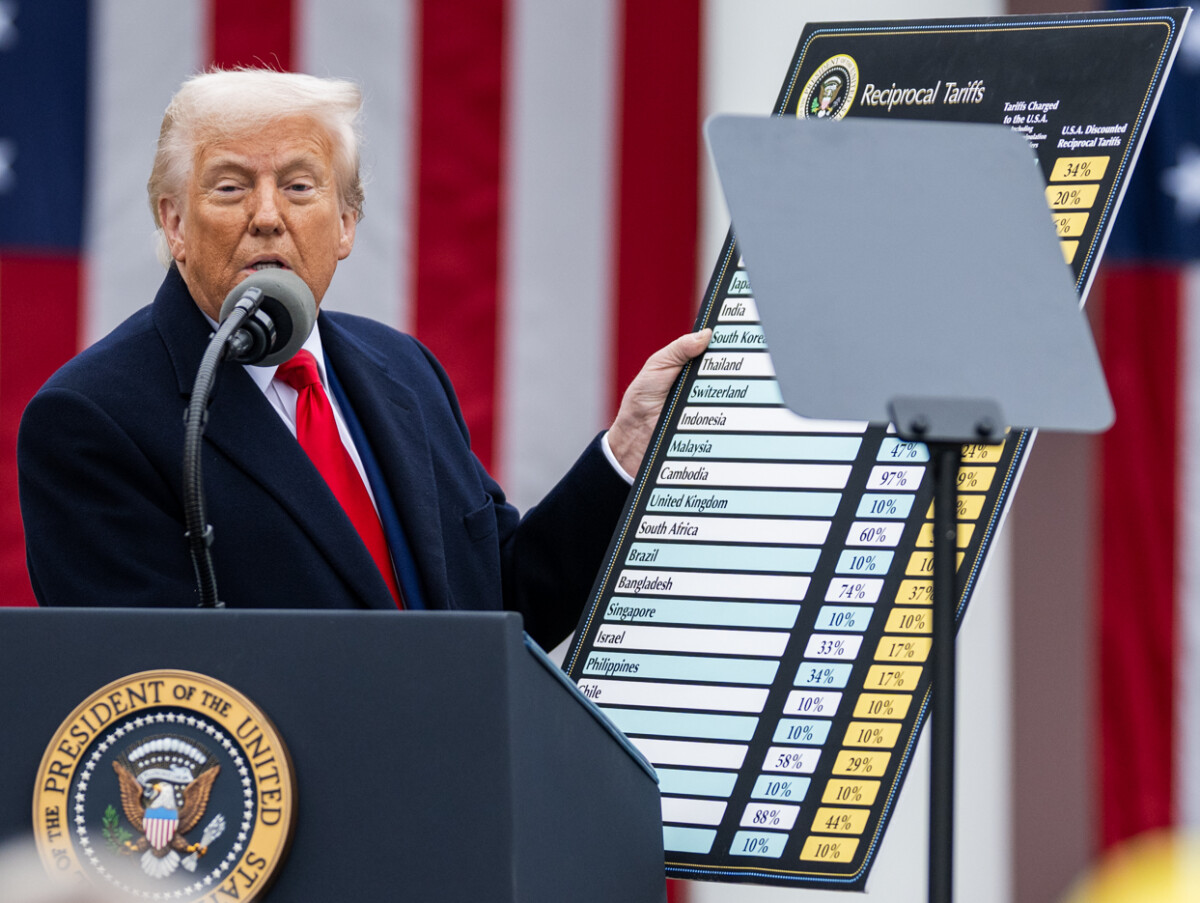
United States: Disparities and Difficult Choices

Elder care in the United States is a patchwork, and many seniors find themselves struggling to get the support they need. The U.S. spends just 1.6% of its GDP on elder care, which is much lower than most developed countries. According to a 2024 report from the National Institute on Aging, nearly 40% of seniors have trouble accessing necessary care—often due to cost, distance, or lack of available services. Without a universal healthcare system, many older adults face high out-of-pocket expenses, forcing some to choose between medical care and other essentials. There’s also a growing shortage of qualified caregivers, which makes the problem worse. While some states have excellent programs, the overall picture is one of inequality and uncertainty for millions of seniors.
Italy: Family Bonds But Systemic Gaps

Italy is famous for its strong family ties, but that alone isn’t enough to ensure quality elder care. The country spends just 2.5% of its GDP on this sector, which is not enough to keep up with its rapidly aging population. According to a 2023 study from the Italian National Institute of Statistics, 30% of seniors have trouble accessing care services, especially outside major cities. Many families end up providing care themselves, often without proper training or support, which can lead to stress and burnout. The healthcare system is stretched thin, and seniors in rural areas are especially vulnerable. While community and family remain important, there’s a pressing need for more resources and coordinated services.
Greece: Economic Struggles Take Their Toll

Greece’s ongoing economic difficulties have hit its elder care system hard. The country allocates only 1.8% of its GDP to elder care, and resources are stretched to the limit. According to the Hellenic Statistical Authority, over 50% of seniors in Greece are living in poverty, making it even harder for them to access the care they need. Much of the burden falls on family members, but without government support or training, many seniors go without essential services. The infrastructure for elder care is limited, and there are few programs to help with social engagement or mental health. The result is a system under strain, with many older Greeks feeling left behind as the population continues to age.